Measles and Rubella – How to Eradicate them?
From Current Affairs Notes for UPSC » Editorials & In-depths » This topic
IAS EXPRESS Vs UPSC Prelims 2024: 85+ questions reflected
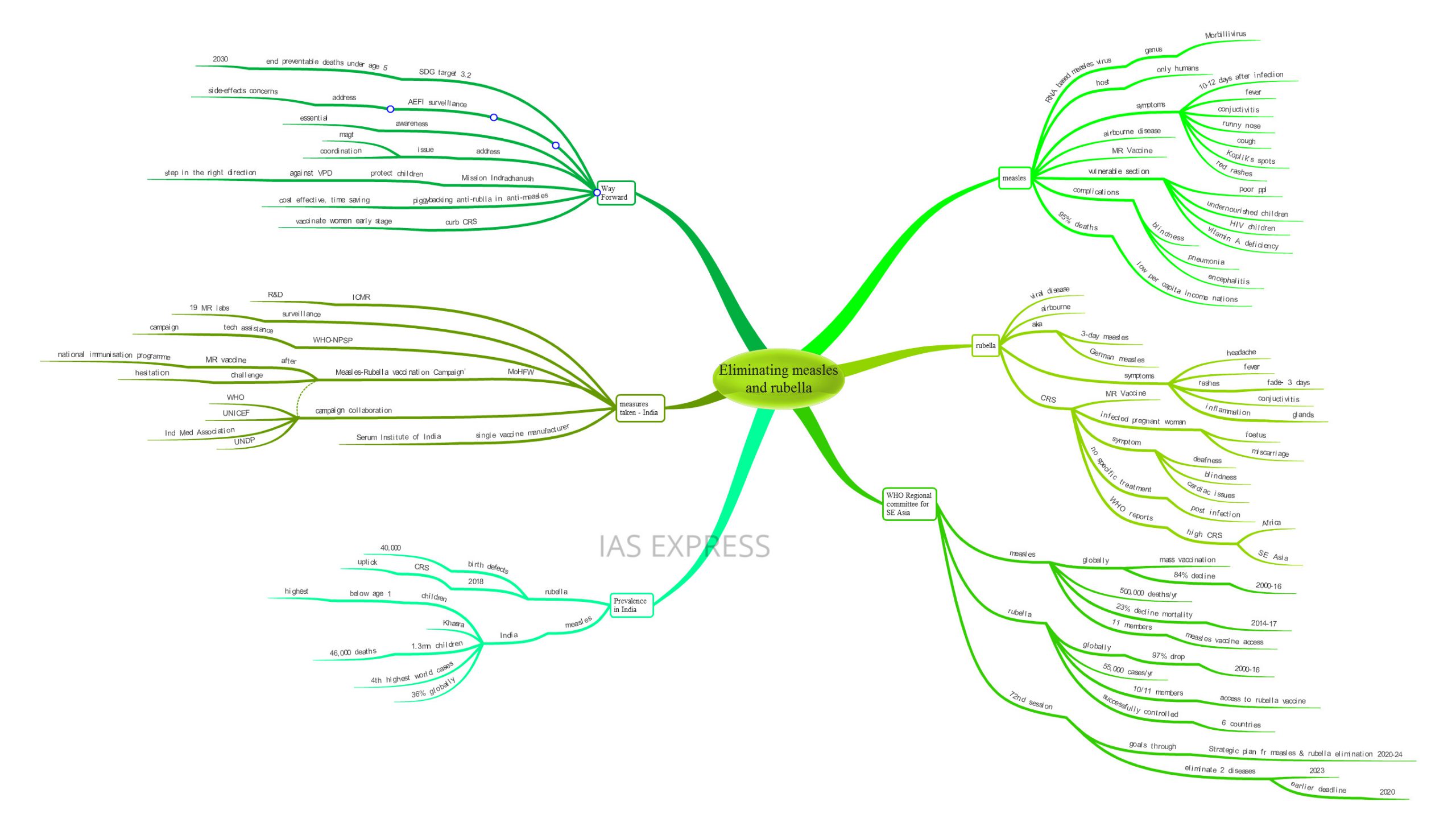
The member nations of the WHO Regional Committee for South-East Asia have postponed the deadline for achieving the eradication of measles and rubella. India accounts for 36% of the global measles cases. The major campaign undertaken by the Indian government is currently facing challenges due to the reluctance of the public and also because of its vast coverage. The deadline has been postponed mainly due to these hindrances. The government needs to address these issues to make India free from the two major childhood killers – measles and rubella
What is Measles?
- Measles is a viral disease caused by RNA based Measles virus of the Morbillivirus
- Humans are the only known host of the virus. It infects 90% of all non-immune individuals upon contact.
- It is an airborne disease that is spread through sneezing, coughing, contact with secretions, close contact with the infected persons, etc. The virus can remain active for even up to 2 hours outside the host.
- Symptoms appear 10 to 12 days after infection. An infected person can spread the disease to others even 4 four days before the onset of the symptomatic rashes.
- Common symptoms of measles include fever, conjunctivitis (inflammation of the eyes), runny nose, cough, Koplik’s spots (white spots inside the mouth), red rashes, etc.
- Innate immunity that is obtained from the mother protects the child for up to 9 months. But this is lost over time and makes the child vulnerable to Measles infection.
- Vaccination is the best way to tackle the disease as current treatments available are only supportive in nature.
- MR (measles and rubella) Vaccine is used widely. 2 doses are given to infants- first between 9 to 15 months and then again between 15 months to 6 years.
- The undernourished children and children affected by HIV are most vulnerable to the disease. Vitamin A deficiency is also connected with the vulnerability.
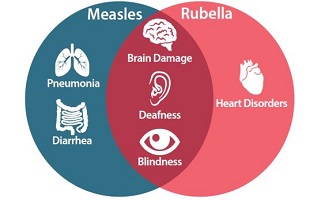
- The disease may cause complications like pneumonia, encephalitis, blindness, etc.
- 95% of measles deaths occur in countries with low per capita income.
What is Rubella?
- Rubella is also a viral disease that is spread through airborne routes.
- It is caused by Rubella virus which is RNA based.
- It also shows rashes as symptoms (like in Measles) and is also known as 3-days Measles or German Measles.
- Symptoms include conjunctivitis, inflammation of glands (like lymph glands), headache, fever, rashes that fade in 3 days, etc.
- Congenital Rubella Syndrome/ CRS occurs in the foetus of an infected pregnant woman as the virus can cross the placenta. Infection during the early stage of pregnancy can cause miscarriage.
- Symptoms of CRS include deafness, blindness, cardiac issues, etc.
- As there is no specific treatment post-infection, vaccination using the MR vaccine is the best option.
- WHO reports that CRS incidence is highest in African and South-east Asian regions.
How is the South-east region dealing with these diseases?
- Measles has been causing 500,000 deaths in the region per year.
- Annually, there are over 55,000 cases of rubella infection in the region every year.
- The region has seen a 23% decline in measles-related mortality between the years 2014 and 2017. Globally, measles-related deaths have dropped by about 84% from 2000 to 2016. Yet 7 million people had been affected by measles in 2016.
- This is due to mass vaccination campaigns. Nearly 366 million children have been covered by it since 2017.
- Globally, Rubella incidence has dropped by 97% between 2000 and 2016.
- Of the 11 member countries, 10 have provided access to rubella vaccination coverage while all 11 have provided access measles vaccination coverage to the children.
- Currently, the 72nd session of the WHO Regional Committee for South-East Asia set the deadline for eliminating these two diseases at 2023.
- This is a postponement of the earlier deadline set at 2020. This is in accordance with the ‘Measles Elimination and Rubella/CRS Control by 2020’ program of the committee. The elimination of these diseases has been the regional committee’s priority since 2014.
- Till date, Bhutan, Sri Lanka, Maldives, Timor Leste, and DPR Korea have succeeded in eliminating Measles.
- Six countries of the region, Nepal, Sri Lanka, Bangladesh, Bhutan, Maldives, and Timor Leste have successfully controlled Rubella incidence among their respective populations.
- The 72nd session’s goals are to be achieved by the use of ‘Strategic Plan for Measles and Rubella Elimination 2020-2024’. This is the roadmap which the countries are to follow to meet the goals by the deadline year.
- The plan involves the use of financial, societal and political support for interrupting the transmission of indigenous viruses (measles and rubella) by 2023.
- The resolution calls for:
- Strengthen the immunisation system
- Sustain high-level population immunity
- Use of sensitive laboratory supported surveillance system
How prevalent are these diseases in India?
- Measles is known as Khasra in India. It is a major issue especially among the poor sections of the population. Undernourished children constitute a major portion of its victims.
- Every year, 1.3 million children acquire the disease every year. Of this, 49,000 children die every year.
- India has the 4th highest number of measles cases in the world. Measles cases from India constitute 36% of the global numbers.
- Children under the age of one have the highest incidence of measles. This is followed by the age brackets 1 to 4 years and 5 to 9 years.
- Every year, Rubella infection has been causing 40,000 cases of birth defects in the country.
- Early 2018 reports showed that the number of CRS cases in India has been seeing an uptick.
How is India dealing with these diseases?
- India has been using mass vaccination campaigns to control both diseases.
- Though India has been providing vaccination against measles from earlier on as a part of the national immunisation program, the anti-rubella vaccine was added as a piggy-back component in 2017.
- In light of the ‘Measles Elimination and Rubella/CRS Control by 2020’ program, India’s health and family welfare ministry had launched the ‘Measles-Rubella vaccination Campaign’.
- The campaign aimed to cover 41 crore children in the age group of 9 months to less than 15 years.
- Over 200 million children have been covered by this campaign.
- The campaign was carried out in a phased manner, with the first phase covering 5 states and the second covering 8 states and UTs. The entire campaign will stretch across 4 phases.
- This phased implementation of the scheme is because India has a single manufacturer of the vaccine: Pune’s Serum Institute of India.
- Schools, health facilities and community centres were used to implement the campaign.
- The WHO-NPSP (National Polio Surveillance Project) provided technical assistance for the campaign’s implementation. NPSP is known for its role in eradicating polio from the country.
- The surveillance part is supported by a network of 19 MR laboratories across the countries. Along with the Indian Council of Medical Research, it is to play a vital role in the R&D part of the campaign.
- The campaign includes collaboration with a number of players like WHO, UNICEF, UNDP, Indian Medical Association, etc.
- After the conclusion of the campaign, the MR vaccine will become a part of the National Immunisation Program.
- However, vaccination hesitancy and the sheer scale of the immunisation program given the huge population has proven to be issues faced by the campaign.
- In January, the Delhi arm of the project saw impediments when over 70 schools refused to undertake the vaccination campaign.
- Hence, India and the other 10 member countries, after consultations have decided to set the new deadline in 2023.
Way forward
- The concept of piggybacking the anti-rubella vaccine onto the prevalent anti-measles vaccine has proven to be a cost-effective and time-saving measure. This is an example to continue and emulate.
- India’s Mission Indradhanush which is to protect children against Vaccination Preventable Diseases/ VPD has been touted as one of the 12 best practices from around the world. This will also prove to be an effective tool for achieving the new deadline as it covers the ‘catch up’ part of the fight against these diseases.
- Other countries of the region had succeeded in eliminating the disease by use of mass vaccinations. Hence the MR vaccination campaign too would be effective.
- After the conclusion of the campaign, the vaccine would be incorporated into the routine vaccination program of the country. Hence the results achieved would become sustainable in the long run.
- The campaign is one of the largest in the world. Hence, issues of coordination and management that come with it are to be addressed.
- Vaccination hesitancy and vaccination refusal continue to be a problem. These arise from mistrust between the caregivers and the health workers, doubts about the procedure or equipment used, source of the vaccines, misinformation, etc. Proper awareness programs are required to eliminate misconceptions and fears about vaccines.
- The campaign itself had provided for an Adverse Events Following Immunization (AEFI) Surveillance program. This will address the concerns from the public about possible side-effects from the vaccination.
- The Delhi incident highlighted the issue of ‘question of consent’. The established global practice is obtaining parents’ permission before vaccination. WHO recognises oral written and implied permissions. India needs to evolve a well-defined procedure to address this concern.
- Since a pregnant woman cannot be vaccinated against rubella, efforts to vaccinate women earlier on must be taken to curb the incidence of CRS. Health infrastructure must be fortified to treat the pregnant women infected by rubella.
- The Sustainable Development Goal target 3.2 seeks to end preventable death of children under 5 by 2030. Winning the fight against these two diseases is needed for achieving this target.
If you like this post, please share your feedback in the comments section below so that we will upload more posts like this.