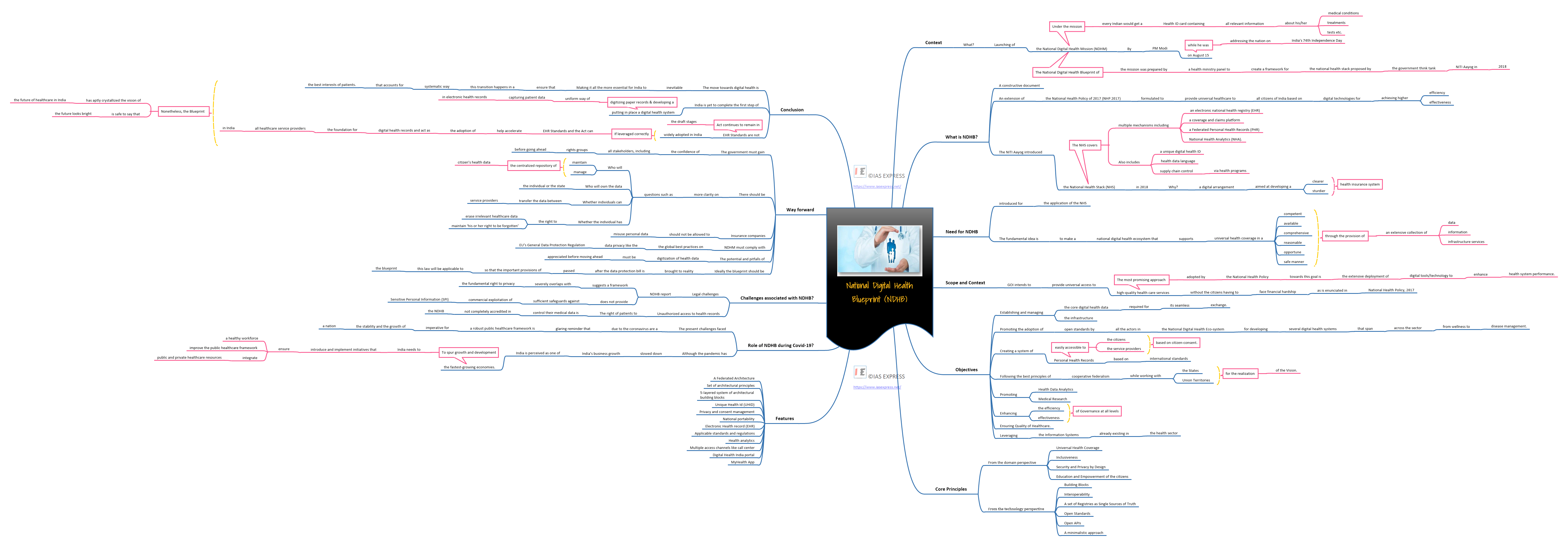
National Digital Health Blueprint – Need, Objectives, Challenges and Way Forward

Recently Prime Minister Narendra Modi has been launched the National Digital Health Mission (NDHM), while he was addressing the nation on India’s 74th Independence Day, an initiative which is completely technology-based and is to revolutionize the health sector in India. The National Digital Health Blueprint of the mission was prepared by a health ministry panel to create a framework for the national health stack proposed by the government think tank – NITI Aayog in 2018. Under the mission, every Indian would get a Health ID card containing all relevant information about his/her medical conditions and treatments, tests etc. For every doctor or a pharmacy, or a lab, they visit, all the detail will be registered in this health card. Ranging from doctor appointment to the medication prescribed, medical tests, when were they done, every bit of detail will be available in your health profile.
Let’s make a detailed analysis of the National Digital Health Mission (NDHM) in this context.
What is mean by National Digital Health Blueprint?
- It is an extension of the National Health Policy of 2017 (NHP 2017) that was formulated to provide universal healthcare to all citizens of India based on digital technologies for achieving higher efficiency and effectiveness.
- The NITI Aayog introduced the National Health Stack (NHS) in 2018, which is a digital arrangement aimed at developing a clearer and sturdier health insurance system.
- The NHS covers multiple mechanisms, including, an Electronic National Health Registry (EHR) that would function as a single foundation of health data for the nation in essence.
- Another mechanism includes coverage and claims platform to function as the building blocks for robust health protection schemes, thereby allowing for the horizontal and vertical expansion of schemes such as Ayushman Bharat by the states, and further allowing a robust system of fraud detection.
- The NHS in addition also aims to provide a Federated Personal Health Records (PHR) system to provide the citizens with access to their health data, and further facilitating the accessibility of the health data for medical research, which is crucial for evolving the understanding of human health.
- Additionally, an interesting mechanism of the NHS includes the introduction of National Health Analytics (NHA). The NHA provides an inclusive data-sharing platform covering various health schemes, and sustaining this platform for smart policymaking and regulation by way of improved techniques, such as, for example, by enhanced projecting analytics.
- To ensure that various aspects of the NHS are fully connected and prevent the accumulation of detached silos, the NHS further includes the introduction of supplementary horizontal systems with a unique digital health ID, health data language, and supply chain control via health programmes.
Need for National Digital Health Blueprint
- The NDHB is a constructive document that has been introduced for the application of the NHS keeping the above initiatives in mind.
- The fundamental idea is to make a national digital health ecosystem that supports universal health coverage in a competent, available, comprehensive, reasonable, opportune, and safe manner, through the provision of an extensive collection of data, information, and infrastructure services.
What is the scope and context for National Digital Health Blueprint?
- Healthcare has always been placed in the centre of all development efforts at a national and global level.
- Government of India intend the attainment of the highest possible level of health and well‐being for all at all ages as its goal
- GOI intends to provide universal access to high-quality health care services without the citizens having to face financial hardship as is enunciated in National Health Policy, 2017.
- The most promising approach adopted by the National Health Policy towards this goal is the extensive deployment of digital tools/technology to enhance health system performance.
- Digital health technology has a huge potential for supporting Universal Health Coverage (UHC) and the government’s commitment to make healthcare affordable, accessible, and equitable.
- There has been an exponential rise in mobile and digital health interventions in India in recent years, with significant public sector resources dedicated to digitizing public health data, often at the source.
- Based on a review of 300 articles in 2018, it was underscored the urgent need for focused research aimed at
- Generating high-quality evidence on the efficacy
- User acceptability
- Cost-effectiveness of mHealth interventions aimed toward health systems strengthening.
What are the objectives of National Digital Health Blueprint?
- The Objectives of NDHB are aligned to the Vision of NHP2017. These objectives are:
- Establishing and managing the core digital health data and the infrastructure required for its seamless exchange.
- Promoting the adoption of open standards by all the actors in the National Digital Health Eco-system, for developing several digital health systems that span across the sector from wellness to disease management.
- Creating a system of Personal Health Records, based on international standards, and easily accessible to the citizens and the service providers, based on citizen-consent.
- Following the best principles of cooperative federalism while working with the States and Union Territories for the realization of the Vision.
- Promoting Health Data Analytics and Medical Research.
- Enhancing the efficiency and effectiveness of Governance at all levels
- Ensuring Quality of Healthcare.
- Leveraging the Information Systems already existing in the health sector
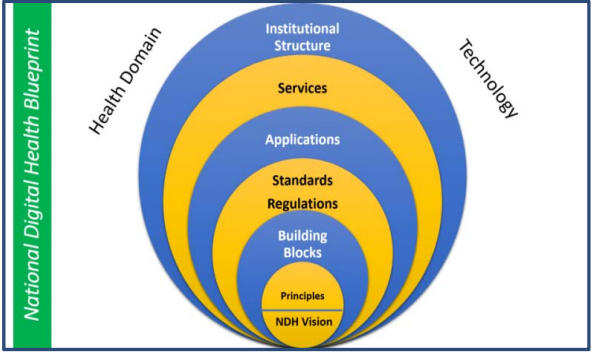
What are the Features of National Digital Health Blueprint?
- The main features of the National Digital Health blueprint include
- A Federated Architecture
- Set of architectural principles
- 5-layered system of architectural building blocks
- Unique Health Id (UHID)
- Privacy and consent management
- National portability
- Electronic Health Record (EHR)
- Applicable standards and regulations
- Health analytics
- Multiple access channels like call centre
- Digital Health India portal
- MyHealth App
Fig: Layered Structures
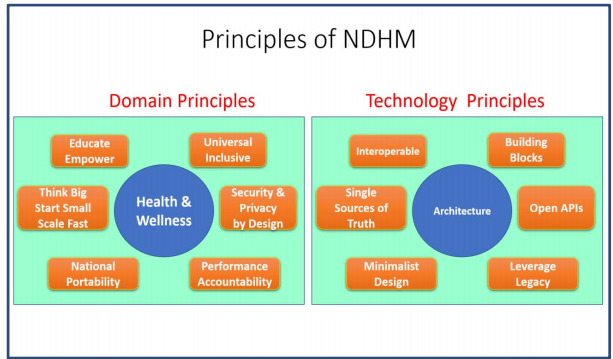
What are the core principles of National Digital Health Blueprint?
- The Core Principles of the Blueprint include
1. From the domain perspective
- Universal Health Coverage
- Inclusiveness
- Security and Privacy by Design
- Education and Empowerment of the citizens
2. From the technology perspective
- Building Blocks
- Interoperability
- A set of Registries as Single Sources of Truth
- Open Standards
- Open APIs
- A minimalistic approach
Fig: Principles of NDHM
What is the role of NDHB during Covid-19?
- India is in critical need of a reliable and affordable framework to manage public healthcare.
- The present challenges faced due to the coronavirus are a glaring reminder that a robust public healthcare framework is imperative for the stability and the growth of a nation.
- Although the pandemic has slowed down India’s business growth, India is perceived as one of the fastest-growing economies.
- To spur growth and development, India needs to introduce and implement initiatives that ensure a healthy workforce, improve the public healthcare framework and most importantly integrate public and private healthcare resources.
- In July 2019, the Ministry of Health and Family Welfare released the National Digital Health Blueprint in the public domain and invited comments from various stakeholders, including the general public.
- This blueprint aims at establishing and managing the core digital health data and provides the appropriate infrastructure required for its continuous exchange.
- This evolution of Indian healthcare can be achieved by supporting the implementation of open standards by all the stakeholders in the National Digital Health ecosystem.
What are the challenges associated with NDHB?
1. Legal challenges
- At a time when the country is right in the middle of a public health emergency, it becomes all the more important to implement the National Digital Health Blueprint to ensure quality care is introduced across all strata of the society.
- However, this implementation comes with an anticipated set of legal challenges.
- One of the main concerns with the National Digital Health Blueprint (NDHB) report is that it suggests a framework that severely overlaps with the fundamental right to privacy.
- Specifically, it does not align fully the privacy principles recommended by the Group of Experts on Privacy (Justice A.P. Shah Committee) and the more recent, Justice B.N. Srikrishna Committee report whose recommendations on data protection form the core foundation for the draft Personal Data Protection Bill, 2018.
- Moreover, the blueprint allows the use of Aadhaar based authentication for schemes under Section 7 of the Aadhaar Act.
- However, the Hon’ble Supreme Court’s Aadhaar judgment held that Aadhaar can be used only when backed by law, and, even the amended Aadhaar Act of 2019 allows Aadhaar to be used only for telecom and banking.
- Additionally, the blueprint does not provide sufficient safeguards against commercial exploitation of Sensitive Personal Information (SPI) that may be caused by private entities that will be linked to public entities under this system.
- These include insurers, pharmaceutical companies, and device manufacturers.
- The use of Aadhaar for online electronic signature service (e-Sign) as a quick and convenient tool to access various medical services under the NDHB framework is an illustrative example of this challenge.
2. Unauthorized access to health records
- The right of patients to control their medical data is not completely accredited in the NDHB, even though the Supreme Court had said in its Privacy Judgment that control over information is a cornerstone of privacy.
- In the absence of concrete legal policy, third parties such as insurance companies, pharmaceutical companies, employers, and data brokers may not be given complete access to the medical data of the patients.
- The present discussion represents just the tip of the iceberg depicting various legal pitfalls associated with the implementation of the NDHB.
- In the present form, there exist serious concerns about the privacy of an individual’s health records. Hence, implementation of the blueprint in the absence of an enforceable data protection law seems impractical.
What could be the way forward?
- The government must gain the confidence of all stakeholders, including rights groups, before going ahead.
- There should be more clarity on questions such as:
- Who will maintain and manage the centralized repository of citizen’s health data
- Who will own the data — the individual or the state
- Whether individuals can transfer the data between service providers
- Whether the individual has the right to erase irrelevant healthcare data and maintain ‘his or her right to be forgotten’
- Insurance companies should not be allowed to misuse personal data.
- The NDHM must comply with the global best practices on data privacy, like the EU’s General Data Protection Regulation.
- The potential and pitfalls of digitization of health data must be appreciated before moving ahead.
- Ideally, the blueprint should be brought to reality after the data protection bill is passed so that the important provisions of this law apply to the blueprint.
Conclusion
- The move towards digital health is inevitable, making it all the more essential for India to ensure that this transition happens in a systematic way that accounts for the best interests of patients.
- The Blueprint may be viewed as more of a long-term goal, which can be operationalised once some of the foundational building blocks have been laid.
- Currently, India is yet to complete the first step of putting in place a digital health system, which is digitizing paper records and developing a uniform way of capturing patient data in electronic health records.
- Once all records have been digitized in a manner that can be accessed across systems, a health information system can be put in place, which would act as a repository for the medical records of every patient.
- The Government has taken certain steps towards prescribing standards for health records and setting up a national health information exchange.
- However, the EHR Standards are not widely adopted in India and the Act continues to remain in the draft stages.
- If leveraged correctly, the EHR Standards and the Act can help accelerate the adoption of digital health records and act as the foundation for all healthcare service providers in India.
- Once these first steps are taken, India can finally move towards the long-term goal of adopting a digital health system envisaged in the Blueprint.
- Nonetheless, the Blueprint has aptly crystallized the vision of the future of healthcare in India, and it is safe to say that the future looks bright.
Practice Question for Mains
- Critically examine the proposed National Digital Health Blueprint. What are the possible implications of it in the health sector of India? (250 Words)
https://www.papertyari.com/general-awareness/national-digital-health-blueprint/
https://main.mohfw.gov.in/sites/default/files/Final%20Report%20-%20Lite%20Version.pdf
https://main.mohfw.gov.in/newshighlights/final-report-national-digital-health-blueprint-ndhb
https://www.nhp.gov.in/NHPfiles/National_Digital_Health_Blueprint_Report_comments_invited.pdf
https://www.medianama.com/2019/08/223-summary-national-digital-health-blueprint-2019/
If you like this post, please share your feedback in the comments section below so that we will upload more posts like this.