National Digital Health Mission – Need, Challenges, Way Ahead

From Current Affairs Notes for UPSC » Editorials & In-depths » This topic
IAS EXPRESS Vs UPSC Prelims 2024: 85+ questions reflected
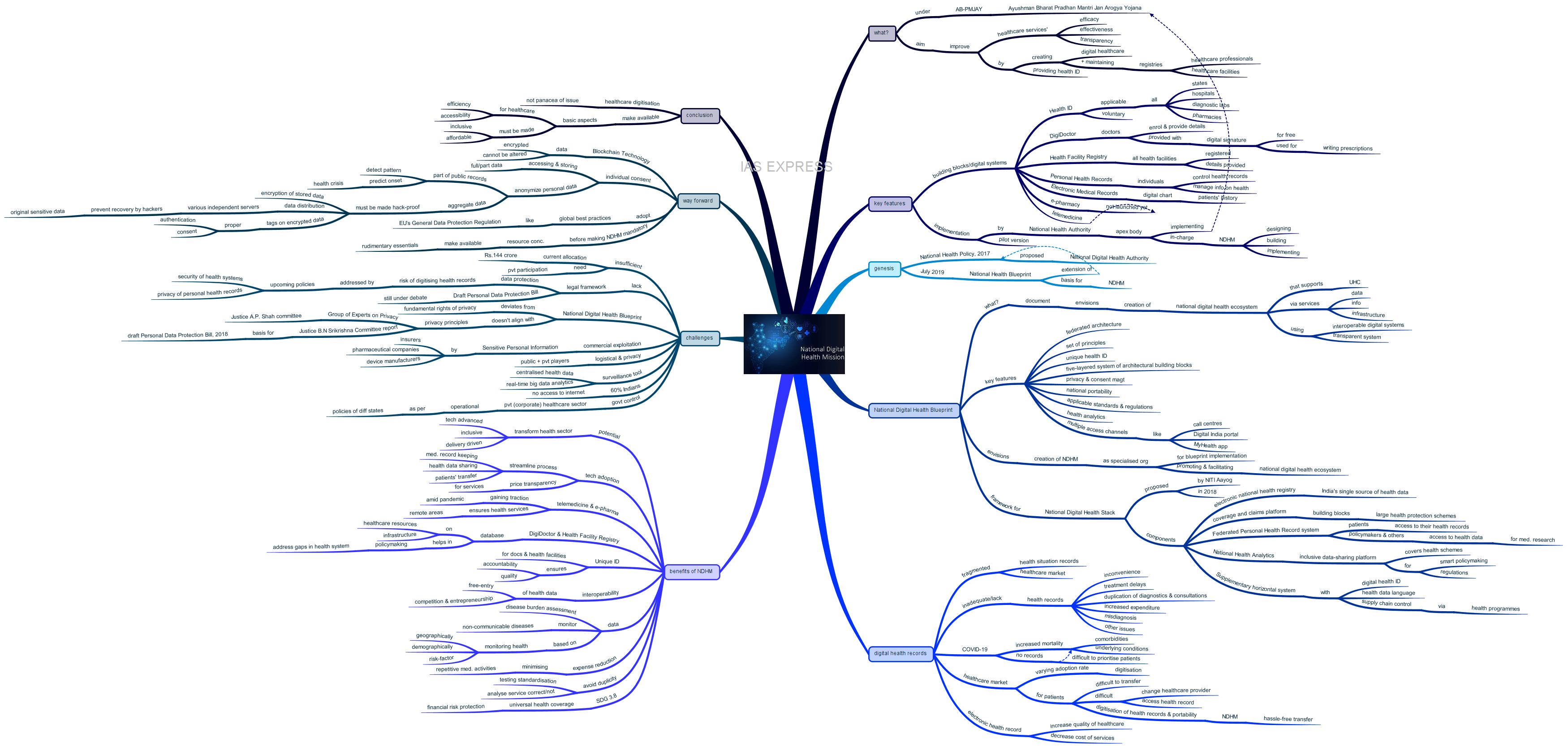
On India’s 74th Independence Day, Prime Minister Narendra Modi unveiled the National Digital Health Mission (NDHM) based on the National Digital Health Blueprint, which was prepared to create a framework for the National Digital Health Stack. With the economic crisis persisting amid the pandemic, India needs to ensure improved and affordable healthcare so as to guarantee a healthy workforce that helps in the recovery process. NDHM is the step in the right direction in this regard. However, the supportive and regulatory aspects must be fortified before the full-scale implementation of the digital healthcare system.
What is the National Digital Health Mission?
- National Digital Health Mission (NDHM), which comes under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), intends to improve the efficacy, effectiveness and transparency of health services in India by creating digital healthcare and creating and maintaining registries for healthcare professionals and facilities.
- Under this initiative, Indian citizens will be provided with a new Aadhaar-like health ID that will store the individual’s medical records, including doctor visits, diseases, the line of treatment and drugs taken.
- It will also integrate various digital health services to create an ecosystem that brings together existing health information systems like telemedicine and e-pharmacy.
What are the key features of the National Digital Health Mission?
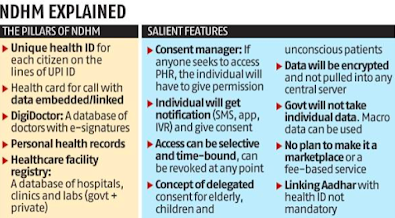
- National Digital Health Mission is a complete health ecosystem with personal health ID for all Indian citizens, digitisation of health record, registry of doctors and health facilities across the country.
- The government launched a platform consisting of the following key building blocks or digital systems:
- Health ID
- DigiDoctor
- Health facility registry
- Personal Health Records
- Electronic Medical Records
- e-Pharmacy
- Telemedicine
- Except for e-Pharmacy and telemedicine, all of the digital products under the initiative are being implemented.
- e-pharmacy and telemedicine will be implemented during the later stages as their guidelines are currently being framed.
- The Health ID provided under this platform would be applicable across all states, hospitals, diagnostic labs and pharmacies within the country.
- The platform is voluntary. Thus, it is up to the individual to enrol on the app.
- DigiDoctor feature in this platform would enable doctors from across the country to enrol and provide details, including their contact information. Those doctors who enrolled in this platform will be provided with a digital signature for free to be used for writing prescriptions.
- Under the Health Facility Registry, all health facilities like hospitals would be registered. Details regarding these facilities would also be recorded in this system, like the services offered, specialities etc.
- Personal Health Records involves individuals controlling their health records and managing information regarding their health.
- Electronic Medical Records is like the digital chart of a patient’s history, treatment records etc.
- National Health Authority, the apex Central Governmental agency responsible for the implementation of Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AM-PMJAY), is in charge of designing, building and implementing the NDHM.
- The mission was rolled out through a pilot launch in 6 union territories – Chandigarh, Ladakh, Dadra and Nagar Haveli, Daman and Diu, Puducherry, Andaman and Nicobar Islands and Lakshadweep.
How did it come to be?
- The NDHM can be traced back to the National Health Policy, 2017 that proposed a new National Digital Health Authority.
- In July 2019, the National Health Blueprint was released by the Union Ministry of Health and Family Welfare, which is the extension of the National Health Policy, 2017.
- National Digital Health Blueprint recommended the setting up of NDHM, a governmental organisation with complete functional autonomy on the lines of UIDAI and Goods and Services Network.
What is the National Digital Health Blueprint?
- National Digital Health Blueprint (NDHB) is a document that envisions the creation of national digital health ecosystem that supports universal health coverage in an efficient, accessible, inclusive, affordable, timely and safe manner, through the provision of a wide range of data, information and infrastructure services using transparent and interoperable digital systems.
- The key features of the blueprints are as follows:
- A federated architecture
- A set of principles
- A five-layered system of architectural building blocks
- A unique health ID (UHID)
- Privacy and consent management
- National portability
- Electronic health records
- Applicable standards and regulations
- Health analytics
- Multiple access channels like call centres, Digital India portal and MyHealth app.
- The blueprint envisions the creation of NDHM as a specialised organisation in charge of implementing it and promoting and facilitating the evolution of national digital health ecosystem.
- This blueprint provides the basis for the application of National Health Stack (NHS)
- Nation Health Stack was introduced by the NITI Aayog in 2018.
- It is a shared digital health infrastructure that aims at ensuring a clearer and sturdier health insurance system.
- It is proposed as India’s first futuristic nationally shared digital healthcare infrastructure usable by both the Centre and state across the public and private sector
- It has the following components:
- Electronic national health registry that is the single source of health data for the nation
- A coverage and claims platform that would serve as the building blocks for large health protection schemes like Ayushman Bharat and enable a robust system of fraud detection
- A Federated Personal Health Record system that would provide access to patients their own health records and the policymakers and others the access to health data for medical research
- National Health Analytics provides an inclusive data-sharing platform covering various health schemes for smart policymaking and regulation by improved techniques
- The supplementary horizontal system with unique digital health ID, health data language and supply chain control via health programmes are included for the implementation of various aspects of National Health Stack in an integrated manner.
Why does India need to digitise health records?
- Records of the health situation and the healthcare market in India are highly fragmented.
- The issue of inadequate record-keeping in public hospitals has been documented in reports by the Comptroller and Auditor General (CAG) of India.
- These revealed instances of hospitals’ failure to even keep records of basic parameters like date, time of consultation, diagnosis etc.
- This lack and inadequacy of uniform records of services received by a patient create inconvenience, duplication of diagnostics and consultations, treatment delays and increased expenditure.
- Loss of records and delays can also cause misdiagnosis and other issues for the patients.
- This issue is especially highlighted during the coronavirus pandemic.
- Mortality from COVID-19 increases by comorbidities or underlying conditions like hypertension and diabetes.
- The lack or poor health records of the COVID-19 patients make it difficult for the doctors to prioritise patients during the times of crisis.
- The healthcare market has a varying adoption rate of digitisation.
- Though few hospitals have voluntarily adopted electronic health records standards notified by the government, it is not possible for patients to digitally transfer their health records from one hospital to another.
- This unfairly confines the patient to the first hospital he/she visited or frequently visits.
- If one needs to change a healthcare provider because of cost or quality concerns, it is highly difficult to have access to health records.
- It is up to the individual to safeguard the pieces of paper consisting of doctor prescriptions and test reports and transfer them from one doctor to another.
- The digitisation of health records and their portability from one healthcare to another would ensure a hassle-free transfer of health records by the patients.
- Studies have shown that the adoption of electronic health records can lead to an increase in the quality of care received by the patients while also decreasing the cost of these services.
What are the benefits of National Digital Health Mission?
- The NDHM has the potential to transform the healthcare sector, making it more technologically advanced, inclusive and delivery-driven.
- The adoption of technology to streamline processes like medical record-keeping, sharing of healthcare data, appointments and other healthcare processes would help citizens to make informed decisions on treatments they receive and prevent their lack of awareness from being exploited.
- It eases the patients’ transfer from one healthcare provider to another and also ensures transparency in the pricing of the services provided within the healthcare sector.
- The telemedicine and e-pharmacy envisioned under NDHM are gaining traction during the on-going pandemic, when patients have limited access to the healthcare providers. They have the ability to provide health services to even those in the remote areas across the country.
- The DigiDoctor and Health Facility Registry ensure that India, for the first time, will have a live and consolidated database of healthcare resources and infrastructure within the country. They will also help in policy planning to address the lacunae in the system.
- Disease burden assessment would be made easy for the policymakers.
- The non-communicable diseases can be easily monitored under this initiative and remedial measures can be given at the earlier stages instead of responding to it at a critical stage.
- Using the available data, the government can ensure the health policies are implemented based on geographical, demographical and risk-factor-based monitoring of health.
- It reduces the expenses on healthcare for patients by minimising the need for repetition of tests and other medical activities while changing the healthcare provider.
- It would ensure avoidance of duplicity of tests by bringing in testing standardisation and help analyse whether the correct care is given to the patient or not.
- Providing unique identification to the doctors and health facilities can ensure quality and accountability of the health services.
- Interoperability of the health data encourages free-entry and facilitates competition and entrepreneurship by small and big players, both in the private and public sector.
- NDHM is a means to achieving Sustainable Development Goal 3.8, which is the universal health coverage, including financial risk protection.
What are the challenges?
- The NDHM is supposed to cover all government health programmes, which is a huge exercise that requires more resources than the current allocation of Rs.144 crore, making private participation inevitable because of the strained exchequer.
- Though the programme has the potential to become a gamechanger, much depends on the implementation and the laws surrounding it.
- India currently lacks a legal framework for data protection in the country, increasing the risk of digitisation of personal health records.
- Draft Personal Data Protection Bill has been under debate for the past 2 years. This proposed bill seeks to protect ‘sensitive data’ related to health, finance, genetics etc.
- The imminent adoption of NDHM in the absence of a data protection law has led the government to plan for two policies – security of health systems and privacy of personal health records.
- These policies take into account the globally accepted norms on privacy by design, risk management and fiduciary principles for building the upcoming digital health records ecosystem.
- The National Health Authority would play an important role in the development of these policies and managing NDHM.
- One of the major concerns with the National Digital Health Blueprint report, based on which the NDHM is built on, is that it suggests a framework that deviates from the fundamental rights of privacy. It does not align with the privacy principles recommended by the Group of Experts on Privacy, Justice A.P. Shah committee and the more recent Justice B.N Srikrishna Committee report, whose recommendations were adopted by the draft Personal Data Protection Bill, 2018.
- There is also the challenge of commercial exploitation of Sensitive Personal Information by insurers, pharmaceutical companies and device manufacturers.
- The NDHM poses considerable logistical challenges and privacy concerns as it involves collaboration between both public and private hospitals, laboratories, insurance firms, pharmacies and telemedicine.
- The implementation of this ambitious architecture technological challenges, considering that 60% of Indians still do not have access to the internet.
- There is also the necessity of digitisation of facilities of all kinds – hospitals, diagnostic centres, pharmacists, among service providers.
- There is a possibility that the NDHM becoming a mandatory exercise in the near future for availing government health services.
- Centralised health data, with real-time big data analytics envisioned in NDHM, creates a possibility of the initiative becoming a surveillance tool.
- There also exists a dilemma for those health service providers who have already adopted a strong and sophisticated software system on whether they have to scrap the existing systems or run a parallel software provided by the NDHM.
- There is also the concern regarding the government control over the private (corporate) healthcare sector that is currently operational as per the policies of different states.
What can be the way forward?
- The ambitious plans of NDHM to create a digital health infrastructure that includes personal health IDs, e-records, telemedicine and e-pharmacy will facilitate inclusive healthcare for all, even for those in the remotest parts of the country.
- It is agreed by the experts that the digitisation of healthcare is the future that needs to be embraced for addressing the shortfalls that currently exists in the sector.
- Yet, while acknowledging the need, it should be taken into account that the health-related data is highly sensitive and its privacy must be protected at all costs.
- Blockchain Technology can guarantee that the data that is created is encrypted and cannot be altered.
- Consent of the individual in accessing and storing data as a part or as a whole must be made mandatory. It can be given by the individual to the trusted authority like a physician, a pharmacy or a research institute as necessary and deemed fit.
- Consent must also be taken to anonymize personal data so that it can be made as a part of public data.
- Healthcare service providers must remove details of the patients that can be used for identifying individuals, especially the medical test results, before sharing it with others who may aggregate it for providing comprehensive statistical data.
- These anonymised indices can be made public to help detect patterns and predict the onset of health crises before they actually arrive for better management.
- In short, while the anonymisation prevents unauthorised personnel from accessing personal data, the aggregation alerts public health authorities on imminent public health issues.
- Even the storage of aggregate data on cloud-servers needs to be made hack-proof.
- This can be done in the following ways:
- Encryption of stored data
- Data distribution across various independent servers to prevent original sensitive data from being recovered by hackers.
- Tags on encrypted data to ensure proper authentication and consent from concerned authorities
- Apart from these, NDHM must also comply with the global best practices on data privacy, like that of EU’s General Data Protection Regulation.
- Like Aadhaar, there is a possibility that the NDHM would become mandatory for availing government health services.
- Before this situation arises, it is necessary to provide for some of the rudimentary essentials like timely care, presence of hygienically maintained healthcare facilities and a decent public health network in addition to other necessary supportive infrastructure like the universal access to the internet.
- The concentration of resources in this front is necessary as no level of digitisation can make up for the absence of such fundamental requirements.
Conclusion
While digital technology can help improve the functioning of the existing health systems within the country, it cannot be the ultimate solution for the existing challenges persisting within the sector. In the absence of basic supportive aspects that ensure efficiency and accessibility of healthcare, the digitisation of healthcare can even backfire, leading to the escalation of existing problems or arising of newer issues. Thus, necessary supportive mechanisms and rudimentary services must be made inclusive and affordable for all before the NDHM is made mandatory in future
Practice question for mains:
What are the challenges that arise during the implementation of the National Digital Health Mission? How can they be addressed? (250 words)
If you like this post, please share your feedback in the comments section below so that we will upload more posts like this.

![[Premium] Surrogacy Regulation in India: The Big-Picture Analysis](https://www.iasexpress.net/wp-content/plugins/pt-content-views-pro/public/assets/images/lazy_image.png)
Nice article
Very organized article