Herd Immunity During Coronavirus Pandemic – Issues And Drawbacks

From Current Affairs Notes for UPSC » Editorials & In-depths » This topic
IAS EXPRESS Vs UPSC Prelims 2024: 85+ questions reflected
UK government is currently facing criticism for implementing “targeted herd immunity” during the early stages of the coronavirus outbreak in the country. This strategy involves allowing people to be infected so that they can gain immunity. The government was forced to abandon this controversial strategy after seeing an increase in pressure on the country’s healthcare system. Now, the death toll has surpassed 30,000 due to COVID-19 in the UK. The World Health Organisation has warned that herd immunity strategy is experimental at best and dangerous at worst. Yet, some experts in India are also considering this strategy as a way to reduce the problems faced by the economy, which is suffering because of the coronavirus pandemic.
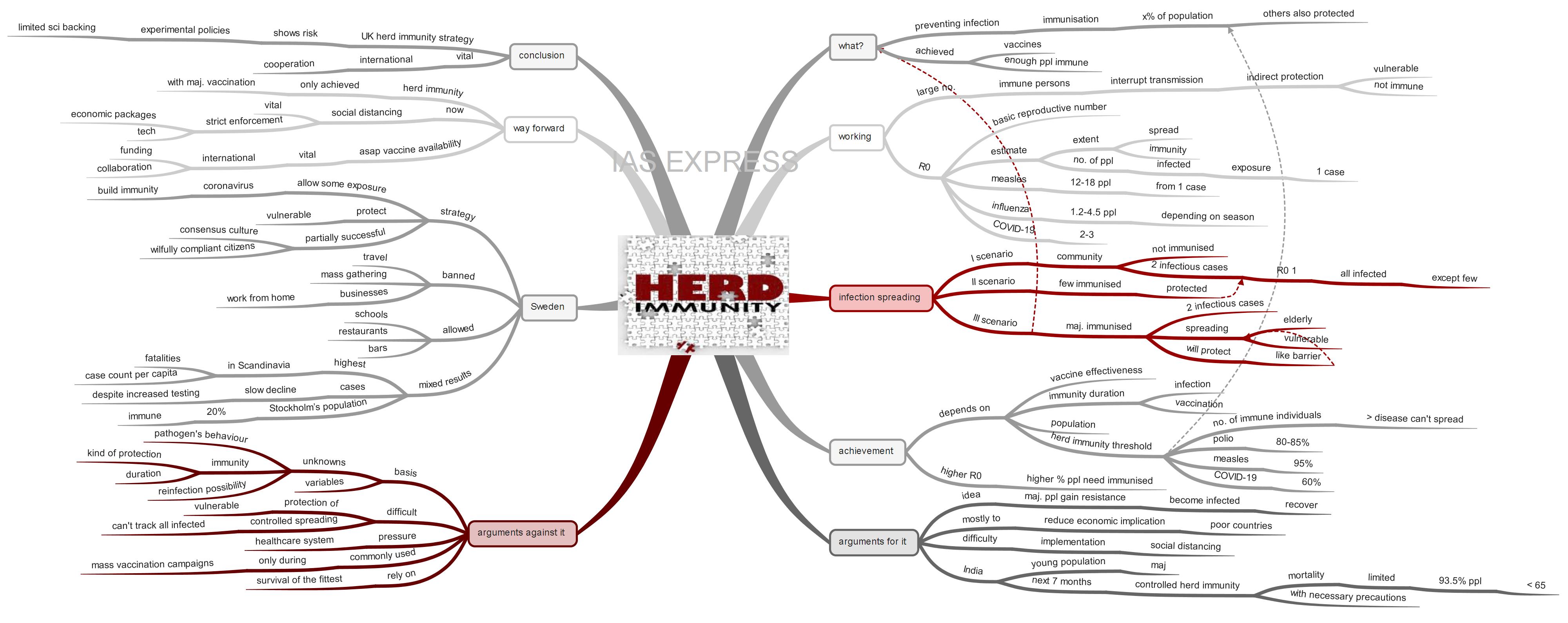
What is herd immunity?
- Herd immunity means preventing an infectious disease from spreading by immunising a certain percentage of the population.
- While this term is mostly used in the context of vaccination, it can also be achieved when enough people have become immune after being infected.
- If a certain percentage of the population is immune to a disease, members of that group can no longer infect another person not belonging to that group.
- This, as a result, would break the chain of infection through the community and prevent infection from reaching those who are the most vulnerable.
- UK government exposing its entire population to the coronavirus infection is under the assumption of the conventional definition that the majority would develop immunity to COVID-19.
How does herd immunity work?
- Herd immunity is based on the scientific principle that the presence of a large number of immune persons in the community, who will interrupt transmission, provides indirect protection to those who are not immune to the infection.
- To estimate the extent of spread and immunity, epidemiologists use a measure called “basic reproductive number” (R0). It indicates how many persons will be infected when exposed to a single case. An R0 of more than one indicates that an individual can spread the infection to multiple persons.
- Scientific evidence indicates that an individual with measles can infect around 12 to 18 persons and a person with influenza can infect around 1.2 to 4.5 persons, depending on the season.
- Based on the evidence available from China, R0 of COVID-19 ranges between 2 and 3.
How does infection spread?
Infection can spread through the following ways:
- The first scenario involves a community that is not immunised. When two infectious cases, both with an R0 value of 1, are introduced, it is highly probable that the whole of the community will be infected, with few exceptions.
- The second scenario involves some people having immunity to the infection. These immunised persons will not be infected when at least two infectious cases are introduced in the community.
- The third scenario is when the majority of the community is immunised. In this case, when two infectious cases are introduced, the spread can take place only among the most vulnerable people like the elderly or other people with weak immunity. Even in such a situation, the immunised persons will protect the non-immunised by acting as a barrier (herd immunity)
When does a community achieve herd immunity?
- It depends on numerous factors like the effectiveness of vaccination, duration of immunity from both the infection and vaccination and the population that transmits the disease.
- Mathematically, it is defined based on a number called “herd immunity threshold”. It is the number of immune individuals above which a disease may no longer circulate.
- The higher the R0, the higher the percentage of the population that has to be immunised to achieve herd immunity.
- Herd immunity threshold of polio is 80-85% and for measles, it is 95%.
- According to the current data, the experts estimate the herd immunity threshold for COVID-19 to over 60%, which means that more than 60% of the population needs to develop immunity to coronavirus to achieve of herd immunity.
What are the arguments for herd immunity in India during coronavirus pandemic?
- The herd immunity strategy allows a majority of the population to gain resistance to the virus by becoming infected and then recovering.
- This radical proposal is mostly advocated to reduce the economic implications of the on-going pandemic-led lockdown.
- It emphasises the challenges the poor developing countries, like Indonesia and some in sub-Saharan Africa, face while implementing lockdown measures.
- India is also facing difficulty while implementing social distancing in crowded living conditions like in many cities and villages.
- Also, no country can afford a prolonged period of lockdown and least of all countries like India.
- A team of researchers at Princeton University and the Centre for Disease Dynamics, Economics and Policy, a public health advocacy group based in New Delhi and Washington, has identified India as a place where the herd immunity strategy can be successful because of its large proportion of the young population.
- According to these experts, unleashing the pathogen in a controlled way for the next seven months would give 60% of India’s population immunity by November, halting the spreading of infection altogether.
- Mortality would be limited as 93.5% of the Indian population is younger than 65.
- These experts recommended the lifting of India’s strict lockdown so that most of the population younger than 60 can return to normal life, though social distancing is still encouraged and other precautions are taken.
- They also urged an increase in the testing during the reopening of the economy.
- This approach has already proven to be controversial internationally as the UK was forced to abandon it at the earlier stage of the pandemic after projections estimated that the healthcare system would be overwhelmed by the increased hospitalisation.
- However, the researchers lobbying for the strategy argue that cultivating herd immunity may be the best of various bad options.
Why herd immunity cannot work against COVID-19 pandemic?
- Using herd immunity at this current juncture would be based on many unknowns and variables.
- Currently, much about the pathogen’s behavior is still not clear.
- There is not enough statistically significant data to estimate conclusively how many individual can get the virus from a single infected person.
- We also don’t know how long the immunity lasts, what kind of protection it offers, whether reinfection is possible.
- It can take months, or even longer, to build immunity against COVID-19. During this time, it would be highly difficult to protect people who are at greater risk – those above 55 years of age and those with co-morbidities like cardiovascular disease and hypertension.
- Allowing virus to infect the population means there will be a sharp spike in the number of patients, putting pressure on existing ICU and emergency beds.
- To prevent healthcare from being over-burdened, it is necessary to slow down the spread of the infection over a large population and flattening the curve. This cannot be achieved by allowing the virus to pass through the entire population.
- It is difficult to undertake “controlled spreading” as it is hard to keep track of all the infected people.
- From the aforementioned arguments, it is evident that this method cannot be used, especially in a country with a huge population like India.
- India, with a population of 1.3 billion, currently has only 0.55 hospital beds per 1,000 people and 48,000 ventilators.
- This strategy is commonly used during mass vaccination campaigns for diseases like measles, which rely on safe and tested vaccines. Trying this with a deadly, new and untreatable disease is a huge risk. This approach is more of a survival of the fittest.
Did Sweden achieve herd immunity?
- Sweden has adopted a strategy that aimed at allowing some exposure to the virus to build immunity among general population while protecting high-risk group.
- This low-enforcement disease-fighting strategy, to some extent, is successful in Sweden as it has wilfully compliant citizens and a consensus culture.
- Though the government of Sweden is advocating for this strategy, the businesses are not actually proceeding as usual. Most travel and mass gatherings are banned and businesses are encouraged to work from home.
- However, restaurants and pubs are still functioning, some of them only with minimal distancing taking place.
- The country is also allowing schools to function normally.
- The results have been mixed, with the country facing the highest fatalities and case count per capita in Scandinavia, but lower than some of its neighbours to the south.
- According to the country’s chief epidemiologist, this strategy appears to be working and that “herd immunity” could be reached in the capital Stockholm in a matter of weeks.
- A sampling and modelling data is indicating that 20% of Stockholm’s population is already immune to the virus.
- Sweden is currently seeing a slow decline in cases, despite the spike in testing for COVID-19.
- However, the mortality rate is high due to the introduction of the virus in elderly care homes.
- While there is a decline in the number of coronavirus cases in the country, the achievement of herd immunity has proven controversial.
- It is a dangerous strategy that puts the elderly and other vulnerable people at a higher risk of becoming critically ill or dying.
What can be the way ahead?
- The Indian government has shown no indication of adopting the herd immunity strategy.
- Herd immunity can be achieved only with the vaccination of the majority of the people.
- Until then, it is best to control the spread of the COVID-19 through social distancing so that all are given the necessary care by the healthcare system.
- Opting for this strategy now, when there are no vaccines, cannot achieve the necessary results.
- Thus, to ensure that the vaccines are available as soon as possible, research for the same will need international funding and collaboration.
- To encourage people to maintain the social distancing norms, it is vital to provide economic packages so that they are not forced to venture out for survival and to use technology to enforce it stringently.
Conclusion:
The UK’s debacle in implementing herd immunity strategy shows the risks of undertaking experimental policies based on limited scientific backing. To eliminate future repetition of the same, the countries needs to overcome their differences, at least during the common crises like a pandemic, to collaborate in scientific research and development so that people’s lives are not risked again.
Practice question for mains:
Government policies to deal with epidemics should be based on scientific evidence and proven measures. Elucidate. (250 words)
If you like this post, please share your feedback in the comments section below so that we will upload more posts like this.