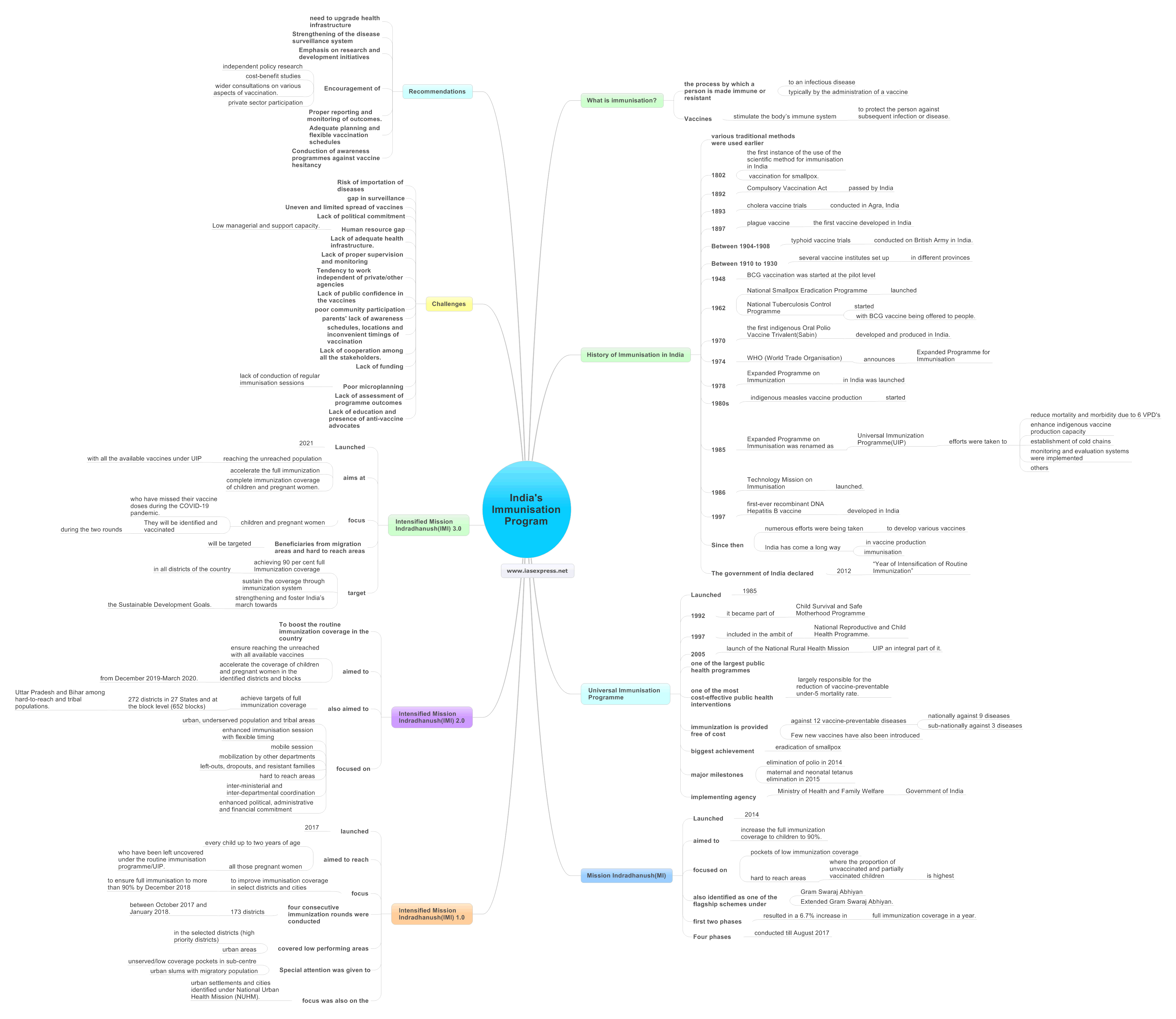
India’s Immunisation Program – History, Schemes, Challenges and Recommendations

From Current Affairs Notes for UPSC » Editorials & In-depths » This topic
IAS EXPRESS Vs UPSC Prelims 2024: 85+ questions reflected
As India is preparing to vaccinate most of its population against the COVID-19 disease, India’s immunisation program and its readiness have come to the fore as a matter of discussion. Immunisation is a proven tool to control and eliminate life-threatening diseases. India has numerous schemes and programs to save its population from various diseases and it has the legacy of adhering to reach the goals it set for itself. The Government of India in collaboration with the States runs various immunisation programs throughout the country and ensures the health and wellness of its population. At the same, the country faces several challenges in delivering vaccines to targeted beneficiaries and thus it will be keenly observed how the nation deals with the challenges in administering its immunisation programs.
What is immunisation?
Immunization is the process by which a person is made immune or resistant to an infectious disease, typically by the administration of a vaccine. Vaccines stimulate the body’s immune system to protect the person against subsequent infection or disease.
History of Immunisation in India
- Although various traditional methods were used earlier, the first instance of the use of the scientific method for immunisation in India was found in 1802 with the vaccination for smallpox.
- In 1892, the Compulsory Vaccination Act was passed by India.
- In 1893, cholera vaccine trials were conducted in Agra, India.
- The plague vaccine was the first vaccine developed in India in 1897.
- Between 1904-1908, typhoid vaccine trials were conducted on British Army in India.
- Between 1910 to 1930, several vaccine institutes set up in different provinces of the country.
- In 1948, BCG vaccination was started at the pilot level.
- In 1962, National Smallpox Eradication Programme was launched. In the same year, National Tuberculosis Control Programme was started with BCG vaccine being offered to people.
- In 1970, the first indigenous Oral Polio Vaccine Trivalent(Sabin) was developed and produced in India.
- In 1974, WHO (World Trade Organisation) announces the Expanded Programme for Immunisation. Following this, Expanded Programme on Immunization in India was launched in 1978.
- In the 1980s, indigenous measles vaccine production was started.
- In 1985, Expanded Programme on Immunisation was renamed as Universal Immunization Programme(UIP) when its reach was expanded beyond urban areas. Under this programme, efforts were taken to reduce mortality and morbidity due to 6 VPD’s, indigenous vaccine production capacity was enhanced, cold chains were established, monitoring and evaluation systems were implemented and others.
- In 1986, Technology Mission on Immunisation was launched.
- In 1997, the first-ever recombinant DNA Hepatitis B vaccine developed in India.
- Since then, numerous efforts were being taken to develop various vaccines against various diseases and India has come a long way in vaccine production and immunisation in India.
- The government of India declared 2012 as the “Year of Intensification of Routine Immunization”.
Universal Immunisation Programme(UIP)
- Launched in 1985, it became part of the Child Survival and Safe Motherhood Programme in 1992.
- In 1997, it was included in the ambit of the National Reproductive and Child Health Programme.
- Since the launch of the National Rural Health Mission in 2005, the Universal Immunisation Programme(UIP) has always been an integral part of it.
- Universal Immunization Programme(UIP) is one of the largest public health programmes targeting close to 2.67 crore newborns and 2.9 crore pregnant women annually.
- It is one of the most cost-effective public health interventions and largely responsible for the reduction of vaccine-preventable under-5 mortality rate.
- Under UIP, immunization is provided free of cost against 12 vaccine-preventable diseases: nationally against 9 diseases – Diphtheria, Pertussis, Tetanus, Polio, Measles, Rubella(a severe form of Childhood Tuberculosis), Hepatitis B and Meningitis & Pneumonia which is caused by Hemophilus Influenza type B and sub-nationally against 3 diseases – Rotavirus diarrhoea, Pneumococcal Pneumonia and Japanese Encephalitis. Japanese Encephalitis vaccine is provided only in endemic districts.
- Few new vaccines have also been introduced under the programme which includes rotavirus vaccine, IPV, adult JE vaccine, pneumococcal conjugate vaccine (PCV) and measles-rubella (MR) vaccine.
- The biggest achievement of the immunization program was the eradication of smallpox. The other two major milestones of UIP have been the elimination of polio in 2014 and maternal and neonatal tetanus elimination in 2015.
- Ministry of Health and Family Welfare, Government of India provides several vaccines to infants, children and pregnant women through the Universal Immunisation Programme.
Mission Indradhanush(MI)
- Launched in December 2014, it aimed to increase the full immunization coverage to children to 90%.
- It focused on pockets of low immunization coverage and hard to reach areas where the proportion of unvaccinated and partially vaccinated children is highest.
- It was also identified as one of the flagship schemes under Gram Swaraj Abhiyan and Extended Gram Swaraj Abhiyan.
- The first two phases of Mission Indradhanush resulted in a 6.7% increase in full immunization coverage in a year.
- Four phases of Mission Indradhanush have been conducted till August 2017 and more than 2.53 crore children and 68 lakh pregnant women have been vaccinated.
Intensified Mission Indradhanush(IMI)1.0
- It was launched in 2017. It aimed to reach every child up to two years of age and all those pregnant women who have been left uncovered under the routine immunisation programme/UIP.
- The focus of the special drive was to improve immunisation coverage in select districts and cities to ensure full immunisation to more than 90% by December 2018.
- Under IMI, four consecutive immunization rounds were conducted for 7 days in 173 districts every month between October 2017 and January 2018.
- It covered low performing areas in the selected districts (high priority districts) and urban areas.
- Special attention was given to unserved/low coverage pockets in sub-centre and urban slums with migratory population.
- The focus was also on the urban settlements and cities identified under National Urban Health Mission (NUHM).
Intensified Mission Indradhanush(IMI) 2.0
- To boost the routine immunization coverage in the country, the Government of India introduced Intensified Mission Indradhanush 2.0.
- The programme aimed to ensure reaching the unreached with all available vaccines and accelerate the coverage of children and pregnant women in the identified districts and blocks from December 2019-March 2020.
- It also aimed to achieve targets of full immunization coverage in 272 districts in 27 States and at the block level (652 blocks) in Uttar Pradesh and Bihar among hard-to-reach and tribal populations.
- The mission focused on urban, underserved population and tribal areas, enhanced immunisation session with flexible timing, mobile session and mobilization by other departments, enhanced focus on left-outs, dropouts, and resistant families and hard to reach areas, inter-ministerial and inter-departmental coordination and enhanced political, administrative and financial commitment, through advocacy and others.
Intensified Mission Indradhanush(IMI) 3.0
- Launched in 2021, the programme aims at reaching the unreached population with all the available vaccines under Universal Immunisation Programme and thereby accelerate the full immunization and complete immunization coverage of children and pregnant women.
- The focus of the Intensified Mission Indradhanush 3.0 will be the children and pregnant women who have missed their vaccine doses during the COVID-19 pandemic. They will be identified and vaccinated during the two rounds. Beneficiaries from migration areas and hard to reach areas will be targeted as they may have missed their vaccine doses during COVID19.
- The present campaign will target achieving 90 per cent full Immunization coverage in all districts of the country and sustain the coverage through immunization system strengthening and foster India’s march towards the Sustainable Development Goals.
Since its first phase, Mission Indradhanushhas have covered 690 districts and vaccinated 37.64 million children and 9.46 million pregnant women.
Challenges
- Risk of importation of diseases from neighbouring countries.
- A gap in surveillance. If not maintained and sustained properly, there will be a risk in future.
- Uneven and limited spread of vaccines across the country.
- Lack of political commitment. India had launched UIP many decades ago but still suffers from the problem of infant mortality and others.
- Human resource gap. Low managerial and support capacity.
- Lack of adequate health infrastructure.
- Lack of proper supervision and monitoring, and delay in taking corrective measures in areas of concern at the government level.
- Tendency to work independent of private/other agencies resulting in either duplication of effort or absence of services in some areas
- Lack of public confidence in the vaccines and immunisation programmes.
- There are other issues like poor community participation, parents’ lack of awareness of the immunisation benefits, schedules, locations and inconvenient timings of vaccination for many people (during working hours) etc.
- Lack of cooperation among all the stakeholders. General lack of inter-sectoral coordination and lack of coordination between state and central governments, resulting in missed opportunities to improve immunisation coverage and quality.
- Lack of funding is another issue.
- Poor microplanning and lack of conduction of regular immunisation sessions
- Lack of assessment of programme outcomes. Problems in recording and records not maintained properly.
- Lack of education and presence of anti-vaccine advocates.
Recommendations
- There is a need to upgrade health infrastructure.
- Strengthening of the disease surveillance system.
- Emphasis on research and development initiatives.
- Encouragement of independent policy research, cost-benefit studies and wider consultations on various aspects of vaccination.
- Encouragement of private sector participation.
- Proper reporting and monitoring of outcomes.
- Adequate planning and flexible vaccination schedules.
- Conduction of awareness programmes against vaccine hesitancy.
Way forward
India is among the major buyers and makers of vaccines, locally as well as globally, and has traditionally aimed at self-reliance in vaccine technologies and production. India’s immunisation programmes have also made great achievements. Yet India needs to counter the various challenges that it faces in reaching its immunisation goal. This can be done only if there is increased funding, cooperation and coordination among various stakeholders. The emerging challenges should be treated as opportunities to learn from the weaknesses and make the country a healthy nation.
Practise question
- Write a note on India’s immunisation programme and its achievements.
If you like this post, please share your feedback in the comments section below so that we will upload more posts like this.